Share
 The management of chronic pain requires the integration of mind and body interventions, strategies to maximise function, interdisciplinary therapy and medications.
The management of chronic pain requires the integration of mind and body interventions, strategies to maximise function, interdisciplinary therapy and medications.
The 12 Pathways To Wellbeing provide a cornerstone of practices to guide these therapies.
Medications form a key part of management and are divided into 2 classes, opioid and non opioid medications. A significant number of individuals do not achieve adequate pain relief or have unwanted side effects with opioid medications ( morphine-like).
However there are other non opioiod medication which can reduce both pain symptoms and the dose of opioids. This article outlines the range of choices available.
These non opioid medications are in 5 separate groups.
- antidepressants,
- analgesics
- anti-inflammatories,
- anticonvulsants,
- muscle relaxants.
It is appropriate to rename these drugs as pain modifying agents as they all influence the pain pathways that contribute to the pain experienced.
How to use these medications
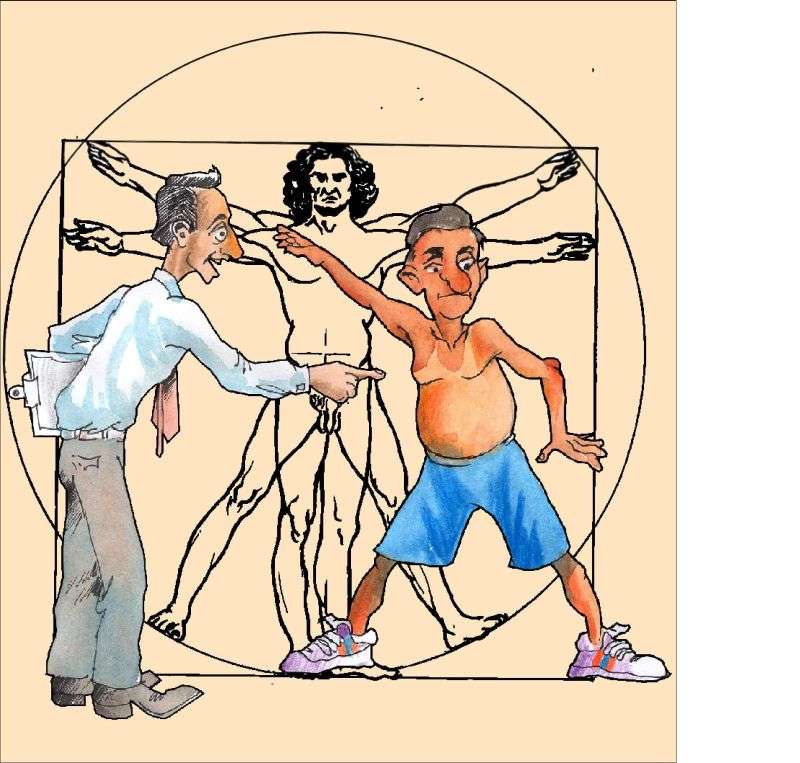
 To achieve the best result a close trusting relationship is necessary with the doctor prescribing the medications.
To achieve the best result a close trusting relationship is necessary with the doctor prescribing the medications.
Both the patient and the prescriber need to be patient and adopt a “start low and go slow approach as there is a risk of unwanted side effects when taking multiple medications.
It is important to make one medication change at any one time and to keep good records. see My Health Organiser.
There are 30 – 40 medications from which to chose.
The best results are achieved with a balanced approach.
