Share
Most people consider that having a scan or xray is the best way to find the cause of their pain and then once this is known …to fix the problem.
This sounds logical until we understand that the human brain is wired to be alert for danger and anything it perceives as a problem activates the alert response.
Seeing a report on a scan that describes “disc bulge” or disc degeneration is often a trigger for the stress response. However if we pause and look at the evidence another interpretation is revealed.
Do you know anyone with a physical problem who has said, “I just want to get an MRI to see what is going on – as there is no harm in that – and I don’t want surgery” ?
Big mistake! Without the ability to evaluate the risks involved in having an MRI, there is the potential for a lot of harm to result. Hence the urgent need to explode the myths around the use of MRIs.
V.O.M.I.T.
In 2003 there was a publication in the British Medical Journal naming a new acronym which was called VOMIT. It is a dreadful name but for a medical condition this commands our attention!
It stands for Victims Of Medical Investigation Technologies.
If we jump to false conclusions the fear response is activated very quickly.
To avoid being a victim, pause to consider what is real and what is imagined on the radiology report and take note of the following.
Exploding The 6 Myths of Using MRIs.
Myth 1 : An MRI can identify the cause of the problem, especially the pain –
There is much research that indicates that MRI scans cannot identify the cause of pain but they are frequently used as if they can.
In fact, having an MRI scan and basing treatment on the scan results alone, can lead to a worse outcome when compared to not having had the scan in the first place.
No matter what area of the body is scanned, spine, knee, or shoulder the results are the same.
Myth 2: There is a direct correlation between the pain and the abnormality of a MRI scan
Individuals with a perfectly normal scan can still have severe and debilitating pain and dysfunction.
Individuals with the most “crappy” looking scans with many abnormalities can have no pain.
The research
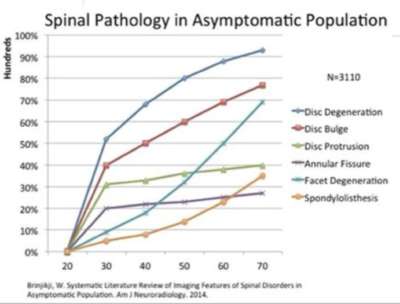
There are many studies that show that up to 20% of individuals under the age of 60 without pain have a disc prolapse on a lumbar spine MRI scan…
And a very significant number of people ( more than 50%) can be shown to have a disc bulge at any age.
60% of individuals with a knee meniscus tear on MRI have no pain or loss of knee function.
The same percentages of MRI abnormalities in individuals without pain can be shown for any joint scanned.
Myth 3: An MRI alone is diagnostic.
The bottom line is that MRI scans do not tell the whole story.
When a MRI is evaluated in the absence of clinical signs and symptoms this can lead to the wrong treatment decision.
A patient who has pain often comes along demanding to have an MRI. When an abnormality is reported he/she draws the conclusion that the scan demonstrates the whole problem. From that point onwards the scan result influences an directs treatment. This can mean inappropriate and unnecessary surgery.
It is therefore very important to seek the advice of a skilled and trusted health professional who do not rely SOLELY on the scan to make diagnoses and treatment decisions.
Myth 4: An MRI can differentiate between an acute injury and a benign pre-existing abnormality.
There are many reports in the literature indicating that if someone has an acute injury and immediately has an MRI scan the recovery is often jeopardised by the existence of an abnormality in the scan whether it is relevant or not.
It is so easy to assume that the scan means something and that this determines the treatment even if the conclusions are wrong. Once the condition of V.O.M.I.T has developed it is difficult to treat. This condition is generally associated with another condition called A.N.T.S. (Automatic negative thoughts). The combination of the combination of these 2 conditions generate anxiety.
A typical example is that an individual who falls over and develops a sudden swollen knee. A MRI scan is done and it shows a torn meniscus. What does this mean and how do we interpret this?
It is possible that the tear was present before the fall.
It is possible that the swelling in the knee is due to trauma in another part of the knee?
Is it really necessary to do an MRI scan just because the knee is swollen?
These are the questions to ask before jumping to the conclusion that surgery is required to treat the torn meniscus.
Another question not often asked is what are the negative long term consequences of surgery? There can be many.
It is relevant to note that doctors themselves are not immune from the persuasiveness of MRI scan abnormalities.
There is a lot of medical information about these uncertainties and dilemmas but it is not repeated often enough.
 Myth 5: Even if you think you are immune from the power of suggestion the very existence of an “abnormal MRI” result can reverberate in your mind and amplify your experience of the problem, especially the pain.
Myth 5: Even if you think you are immune from the power of suggestion the very existence of an “abnormal MRI” result can reverberate in your mind and amplify your experience of the problem, especially the pain.
Most people are familiar with the term placebo. That is, if you take a sugar pill assuming that it is a strong pain relieving medication you have a very high probability of having pain relief.
Most of us however are not aware of the term nocebo. If you see something that you perceive is potentially threatening or a danger to health or is possibly the cause of pain, the brain’s defensive mechanisms will take appropriate defensive responses.
Even if there is no threat, the perception of the threat can lead to a sustained response.
For example, if you have an MRI scan which shows a bulging disc and some authority such as a health practitioner tells you that the bulge is the cause of your problem it is likely that your experience of pain will increase.
There has been a lot written about this issue from this perspective of neuroscience. For example, there is a well- explained book called Explain Pain an a TED talk by Dr Lorimer Moseley from South Australia called “Why Things Hurt” which explains very well the pain system.
More recent books by Norman Doidge, The Brain that Changes Itself and How the Brain Heals demonstrates how self-management strategies can change the way the brain functions.
These and many other resources confirm that anxiety levels are driven by anticipating negative outcomes and these, in turn, amplify the pain experience.
So the seeds of fear for the future find fertile ground in the description of MRI abnormalities when interpreted alone and conveyed as :
“You have nerve root impingement”
“You have a disc prolapse”
“You have a ligament tear
“You have cartilage loss”
“ There is bone on bone in your knee”
All of these statements change an individual’s view of their body and drives the nocebo effect.
Myth 6. An abnormal MRI is an indication for surgery.
As mentioned previously doctors themselves are not immune from the persuasiveness of MRI scan abnormalities. In any region of the body there is a high incidence of MRI abnormalities. If a doctor wants an excuse to operate the best thing they can do is order an MRI scan.
In a newspaper article published in May 2019 the journalist looked at the management of back pain in ballet dancers at the Australian Ballet Company. They applied the principles of pain science to those wh0 developed soft tissue injuries. They avoided scans and in doing so avoided the developments of VOMIT and ANTS in their dancers.
It is very important to read this. Here is the article.
CONCLUSION
 After evaluating a large body of relevant research my view is… that MRI scans have an excellent place in management but they represent only one part of the decision-making process that goes into making a diagnosis and treatment plan.
After evaluating a large body of relevant research my view is… that MRI scans have an excellent place in management but they represent only one part of the decision-making process that goes into making a diagnosis and treatment plan.
The take-home message is :
Consider not having an MRI scan or xrays unless you have a trusted expert on hand who is able to assess your problem based on weighing-up different forms of evidence. Often the best advice is to not have a scan.
Avoid becoming a V.I.C.T.I.M.

