Share

FOOD IS MEDICINE – AN ANTI-INFLAMMATORY DIET
By Dr Daniel Lewis, Rheumatologist
Inflammation is both good and bad.
Acute inflammation is essential for metabolic regulation and the healing of injuries.
It is a response of the immune system to injury, infection, radiation exposure, the influence of toxins, or the activation of autoimmune responses.
The inflammatory process is designed to remove damaged cells, invading pathogens or chemical toxins.
On the other hand, chronic inflammation contributes to and may be the cause of most chronic conditions. This is the condition where there is a prolonged inflammatory response and the original triggering event such as bacterial and viral infections and/or chemical exposure have not been resolved and the inflammatory response continues unchecked.
Over time many different cells in the immune system are activated at the site of inflammation which causes uncoordinated destruction and repair of tissues.
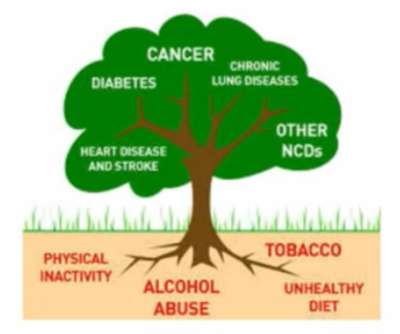
Worldwide 63% of all deaths are due to non-communicable chronic diseases.
Inflammation is a central aspect of most ill health issues.
All of us have some degree of inflammation and the body is well-tuned to deal with it.
Gaining weight and living with stress are just two of the many factors that increase inflammation.
Atherosclerosis, diabetes, osteoarthritis, obesity, stroke, cancer, inflammatory bowel diseases, chronic respiratory diseases, neurological diseases, and all autoimmune diseases are diseases of chronic inflammation.
It is likely that fibromyalgia, central sensitisation, depression, and chronic fatigue illnesses are driven in part by chronic brain inflammation (neuroinflammation).
How to measure inflammation

There are a variety of blood tests that can measure the body load of inflammation. The most common one which in general measures the amount of inflammation occurring in the last 72 hours is called C-reactive protein (CRP). The erythrocyte sedimentation rate(ESR) measures inflammation that has occurred over the last month.
These measures of inflammation do not occur in every individual and there are multiple ways of measuring inflammation.
Up to 30% of individuals can have inflammation and yet these two blood tests are normal.
To measure inflammation, it is necessary to work with your health practitioner to find a test that is relevant to you.
What causes inflammation
- visceral obesity
- poor diet ie. sugar, processed foods, vegetable oils
- lack of exercise
- lack of sunlight
- lack of sleep
- stress
- smoking
- excessive alcohol
What to eat
All of us have some degree of inflammation all the time and the body is well-tuned to deal with it.
Is there one diet that works for all? Nutrition is very individual. What works for you might not work for somebody else. The diet that gets you healthy might not necessarily keep you healthy.
Every diet that is based on
- predominately whole foods (avoiding processed foods)
- low in foods that increase blood glucose levels
- no processed vegetable oils
has been shown to reduced C-reactive protein levels.
- Mediterranean diet
- Nordic diet
- DASH diet
- Low Carb High Fat (LCHF)
- Ketogenic diet

The common denominator in all these diets is that they reduce visceral fat. Most studies comparing these different diets reported a similar decrease in the CRP indicating that weight loss rather than the dietary composition was the primary cause for the reduction in inflammation.
What is visceral fat?
Visceral fat is body fat that is stored within the abdominal cavity and is therefore stored around a number of important internal organs such as the liver, pancreas and intestines. … Storing higher amounts of visceral fat is associated with an increased risk of a number of health problems including type 2 diabetes. Visceral fat also produces increased inflammatory markers.
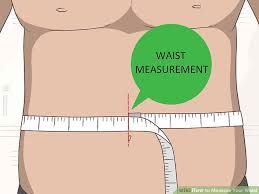 An easy way to measure visceral fat levels can be found by looking at your belly and waist size. If it’s protruding, you likely have a store of visceral fat.
An easy way to measure visceral fat levels can be found by looking at your belly and waist size. If it’s protruding, you likely have a store of visceral fat.
There are 2 ways to assess this
Healthy Waist to Height Ratio (WHrtR) To measure the WHtR, simply record waist circumference, then divide that number by height. A WHtR > 0.5 indicates a higher risk of diabetes, heart disease, stroke and lower life span. A WHtR < 0.5 is a healthy range.
Healthy Waist to hip ratio Your waist to hip ratio estimates the fat distribution in your body. Find out how this can affect your overall health with this interactive tool.
Gaining weight and living with stress are just two of the many factors that increase inflammation.
FOODS TO INCLUDE
There are many foods that can play an important role in an “anti-inflammatory diet.” Here is an overview:
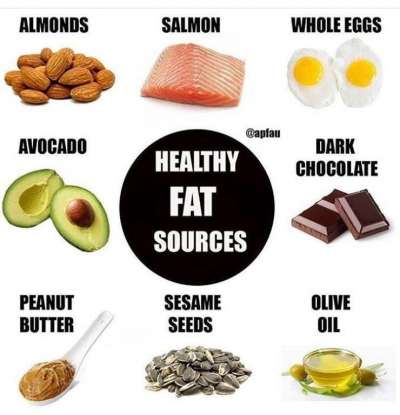
Foods rich in omega-3 fatty acids are considered anti-inflammatory. Foods include:
- fish such as fresh salmon, sardines, tuna, and other cold-water fish; Canned fish is devoid of omega 3. Wild Alaskan salmon or sustainably farmed smoked NZ salmon is high in Omega 3. Unfortunately, farmed salmon which is all that is available in Australia has little omega 3 and mostly omega 6.
- nuts and seeds, notably flaxseeds, hemp seeds and walnuts;
- winter squash and purslane (edible weed). red leaf lettuce
Eggs
The fatty acid composition of free-range eggs has an omega 3: omega 6 ratio of 3: 1. Factory farm eggs are 9:19.
Fat
Extra virgin oil is another food that contains healthy fats (monounsaturated fats), and one that has been found to have anti-inflammatory benefits.
Some of these benefits seem to come through its unique antioxidant phytonutrients, such as oleuropein and hydroxytyrosol.
It’s important to note that these phytonutrients are more concentrated in extra virgin olive than other types of olive oil.
Have these oils ( room temperature) as part of dressing on food. They lose some of their health benefits when heated to high temperatures such as frying.
For lightly frying food use oils with a high smoking point such as coconut oil, avocado oil or macadamia oil. Only high-quality fresh virgin olive oil has a high smoking point. It is best to use other oils for frying.
Do not use vegetable or seed oils ( eg Corn, sunflower or soybean oil) as at high temperatures toxic compounds can be produced.
Saturated fat
These fats include butter, meat fat, coconut oil. Medical research is uncertain as to the direct impact that these fats have on inflammation. There are mixed reports and no clear advice can be given at this time. However, eating fat as part of a ketogenic diet leads to the production of ketone bodies which are anti-inflammatory.
 Cocoa and Coca-rich foods.
Cocoa and Coca-rich foods.
This reduces low-grade inflammation. Must be very low in sugar for benefit.
Dairy
There is no definitive answer as to whether dairy products alone reduce inflammation. It appears they are anti-inflammatory in individuals with metabolic disorders but pro-inflammatory in those with sensitivities to cow’s milk.
Flavonoid, polyphenols and carotenoid phytonutrients
These have strong anti-inflammatory and antioxidant properties. These foods include
deep coloured fruits and vegetables eg berries, cherries, beets, leafy greens, and other richly coloured foods.
Pineapple also contains a proteolytic (protein-digesting) enzyme called bromelain that has anti-inflammatory activity. On the other hand it contains a lot of sugar and many individuals require a low carbohydrate diet to control the risk of diabetes and obesity. Fruits high in sugar need to be avoided.
Dark leafy greens such as kale, spinach, collard greens and swiss chard contain antioxidants, flavonoids, carotenoids, and vitamin C —all of which help protect against cellular damage.
 Tea and Coffee
Tea and Coffee
Green tea and black tea reduces inflammation. It is a healthy antioxidant.
Matcha tea is the most nutrient-rich green tea and comes in the form of a stone-ground unfermented powder. The best Matcha comes from Japan and has up to 17 times the antioxidants of wild blueberries, and seven times more than dark chocolate.
Coffee, which contains polyphenols and other anti-inflammatory compounds, may protect against inflammation, as well.
Tulsi is another tea loaded with anti-inflammatory antioxidants and other micronutrients that support immune function and heart health.
Raw or Cooked vegetables
Aim to eat some vegetables raw and juicing is an excellent way to get more greens into your diet. Have a mixture of lightly steamed greens and raw vegetables.
Juicing high sugar vegetables like carrot and beetroot increase blood sugar levels due to their high fructose and should not be juiced. The same goes for any fruit which must not be juiced.
A glass of orange juice contains 7 teaspoons of sugar. It is not a health food!
Lectins

Lectins are proteins that are found in high quantities in grains, beans, and certain fruits and vegetables. These proteins are made by plants as a defense mechanism against predators.
Whether lectins cause inflammation in humans remains controversial.
High fibre foods:
Reduces bowel inflammation and inflammation in general. If you are overweight, which causes inflammation it is essential to add extra fibre to the diet… it works!
Fermented foods:
There is definitive scientific evidence that gut bacteria are important for a well-functioning immune system.
It is becoming increasingly certain that many inflammatory diseases begin in the gut due to an imbalanced microbiome (dysbiosis).
Fermented foods such as kefir, natto, kimchee, miso, tempeh, pickles, sauerkraut, olives, and other fermented foods such as garlic helps to maintain the beneficial gut bacteria.
Herbs and Spices:
The top 5 herbs and spices that reduce inflammation – Cloves, turmeric, ginger, rosemary, Boswellia serrata.
Probiotics and Prebiotics and the microbiome:
The microbiome is the name that describes all the bacteria in the bowel. A balanced microbiome promotes health.
An imbalanced bacterial load, called dysbiosis is associated with many diseases including autoimmune diseases.
Prebiotics nourish and promote the growth of the “good” bacteria in the bowel.
Prebiotics are a specific form of carbohydrate called fructans. They promote health, reduce constipation, decrease the numbers of pathogenic “bad” bacteria, increase the absorption of calcium, lower triglyceride levels. They modulate insulin and glucagon levels.
One form of prebiotic is called Inulin. Inulin is found in asparagus, leek, onions, bananas and garlic. It stimulates the growth of beneficial intestinal bacteria.
It is a commercially available powder that is taste free and can be added to food.
Specific foods:
Strong anti-inflammatory properties are present in a variety of common foods.
These include;
onion, oregano, red sweet potato, oyster, shitake, enoki mushrooms and cinnamon,
lime zest, English breakfast tea, honey-brown mushroom, button mushroom, raw oyster, shiitake and enoki mushrooms, and cloves.
Anti Inflammatory Supplements

In addition to eating an anti-inflammatory diet, the following herbs and supplements have anti-inflammatory effects.
As research information flows through we will add to this list.
Ginger (Zingiber officinale). Dried, powdered ginger is a potent anti-inflammatory agent, and capsules are readily available in health food stores. Start with one gram per day (usually two capsules), taken after a meal. Occasionally this can cause stomach irritation. There is no toxicity and you can stay on it indefinitely. Add ginger to food and drink for added benefit.
Turmeric (Curcuma longa). This herb is often used in curries. Turmeric has anti-inflammatory properties. This bright yellow spice may also have a specific preventive effect against Alzheimer’s disease and reduce the risk of cancer. Curcumin capsules are more potent than the spice powder. 2000mg/day is the optimal dose.
Potential risks of curcumin (tumeric): It is advised not to take tumeric if you have gallbladder disease. Do not take in the preoperative period as it does lead to blood thinning. Medical advice is required if you are on blood thinning medication. It is not safe in pregnancy and while breastfeeding.
Fish oil. Liquid oil or capsules are the most potent of all forms of anti-inflammatory supplement. It takes 6 to 8 weeks for anti-inflammatory effect maximum effect. It is important to read the small print on the label of each brand and note the level of EPA. For maximum anti-inflammatory effect 2000mg of EPA per day is necessary. It is possible to purchase capsules that have 500 mg EPA per capsule and therefore 4 capsules are needed per day.
Boswellia Serrata 100-250mg/day reduces pain.
There is increasing evidence that a low carbohydrate, high fat, ketogenic diet is an anti-inflammatory diet. In 2016 the evidence is building but not certain. Watch this space. This is what we know so far
Turning the food pyramide upside down.
Foods that change the microbiome and inflammation
Latest research artticle Microbiome and food
Foods to avoid are those that promote inflammation.
SUGAR ( Glucose) It is in capital letters for a reason! Beware sugar is hidden in everything processed. Sweet sugary beverages are known to increase CRP levels.
Sugar includes agave, lollies, chocolate (less than 85% cocoa), corn syrup, fructose, high fructose corn syrup, honey, maple syrup, molasses, sucrose, coconut sugar.
 Most simple carbohydrates and process foods immediately once digested convert to glucose. Recent studies indicate that the conversion of carbohydrate to glucose is dependent on an individual’s gut microbiome one individual can eat a slice of bread and have a massive spike in blood glucose levels whereas another individual will have no effect. It is now possible without too much difficulty to test this in everyone.
Most simple carbohydrates and process foods immediately once digested convert to glucose. Recent studies indicate that the conversion of carbohydrate to glucose is dependent on an individual’s gut microbiome one individual can eat a slice of bread and have a massive spike in blood glucose levels whereas another individual will have no effect. It is now possible without too much difficulty to test this in everyone.
It is possible to look up the glycaemic index and the glycaemic load index to determine which of the foods are likely to stimulate glucose production.
What about fruit?
The sugar in fruit ( natural ) is sugar. High Glycaemic Fruits: including bananas, canned fruits, dried fruits, mango, pineapple, raisins. Eating grapes is known to cause a massive glucose spike in the blood.
Vegetable oils
Sunflower oil, cottonseed, safflower and corn oils may promote inflammation as they are rich in omega-6 fatty acids; Too much omega 6 increases inflammation. Our western diets contain huge amounts of omega 6.
Gluten
A protein called gliadin induces an inflammatory response in individuals who have a condition called coeliac disease. Foods that contain gluten include “White foods” such as white flour, white rice and white sugar;
Although still controversial, there is an increasing recognition that many individuals have a sensitivity to gluten which can induce an immune response and an inflammatory response.
If you have inflammation, a trial of not eating gluten and corn may be very beneficial. There are many links to eating a FODMAP diet which removes many types of carbohydrates that can be associated with food sensitivities.
Gluten-Containing Compounds:
barbecue sauce, binders, bouillon, brewer’s yeast, cold cut meats, condiments, emulsifiers, fillers, chewing gum, hot dogs, hydrolyzed plant and vegetable protein, ketchup, soy sauce, lunch meats, malt and malt flavoring, malt vinegar, matzo, modified food starch, monosodium glutamate, non-dairy creamer, processed salad dressings, stabilizers, teriyaki sauce, textured vegetable protein and some spice mixes.
WGA – Wheat germ Agglutinin.
WGA is not associated with gluten. White bread contains gluten but not WGA. Whole wheat bread contains both.
WGA is a very small protein and can stimulate inflammation. In some individuals, it has been shown to promote inflammation.
Processed foods
 These are foods that contain synthetic flavourings, colourings and preservatives such as cereals, canned foods with high sodium content.
These are foods that contain synthetic flavourings, colourings and preservatives such as cereals, canned foods with high sodium content.
Fructose is found in many fruits and the effect is magnified if fruits are juiced. Orange juice is standard fare in any place where breakfast is served. Hospitals, airlines….The list is endless
Barbequed meats
Margarine and hydrogenated oils
Foods that sometimes cause inflammation ( This is a complex issue and one that requires trial and error)
Dairy: In some individuals dairy is a pro-inflammatory food.
This including butter, cheeses, cow milk, creams, frozen desserts, goat milk, margarine, mayonnaise, sheep milk, whey, yogurt
Nuts and seeds including almonds, peanuts, sunflower seeds, sesame seeds
Grains: including amaranth, barley, buckwheat, bulgur, corn, couscous, kamut, millet, oats, quinoa, rice, rye, spelt, wheat, wheat germ.
Alcohol is a carbohydrate and converts to sugar .
READING FOOD LABELS AND SOME RESOURCES
To eat well you need to have the right food at hand. A priority is to read and understand food labels.
If you see these items on a food label, leave it on the shelf.
Sugar – Especially if it is the number one item on the food list
Artificial sweeteners or non-nutritive sweeteners
Oils – corn, safflower, sunflower, soybean, cottonseed, palm, partially hydrogenated,
Margarine
High fructose corn syrup (HFCS)
Highly recommended books and websites to get you started on an anti-inflammatory way of eating.
 Anti- inflammatory EatingFrom BJG Health.
Anti- inflammatory EatingFrom BJG Health.
 The Autoimmune Solution by Amy Myers
The Autoimmune Solution by Amy Myers
 The Wahls Protocol By Terry Wahls.
The Wahls Protocol By Terry Wahls.
Podcast and website
The bottom line
There is convincing evidence that sugar, refined grains, omega 6 fatty acids and visceral obesity cause and contribute to inflammation.
A whole-food, unprocessed diet, high in vegetables, omega 3 fatty acids, fibre, flavonoids and fermented foods suppress inflammation.
There are many foods that can play an important role in an “anti-inflammatory diet.” Here is an overview:
There is also a significant benefit to focusing on how you eat as being as important as what you eat. There are substantial health benefits by eating mindfully and chewing slowly.
Precision medicine which determines the right nutrition for each person is coming.
To get recipes type into Google AN AUTOIMMUNE PALEO DIET.
these will exclude the following ingredients:
- Food additives
- Processed foods
- Refined sugar,
- Refined seed oils
- Grains and corn), dried legumes (including soy),
- Fesh legumes such as green beans and peas
- Dried legumes and this includes soy
- Eggs
- Nuts and seeds – this includes nut butter and nut milk
- Dairy
- Nightshade vegetables.
- Spices
- Herbs are OK.