Share
 The diagnostic criteria for ME/CSF are now almost 30 years old and mostly the diagnosis depends on an individual’s report of symptoms and function. There are still no specific biomarkers for diagnosis.
The diagnostic criteria for ME/CSF are now almost 30 years old and mostly the diagnosis depends on an individual’s report of symptoms and function. There are still no specific biomarkers for diagnosis.
There are three criteria widely used to define ME/CFS patients: Fukuda (1994), Canadian Consensus Criteria (2003) (CCC) and the International Consensus Criteria (2011) (ICC).
The search for easy-to-measure biomarkers continues. There are many complex biochemical abnormalities that are commonly found but there remains no simple test to confirm the diagnosis. There are no simple or reliable treatments that assist individuals to regain their energy and function.
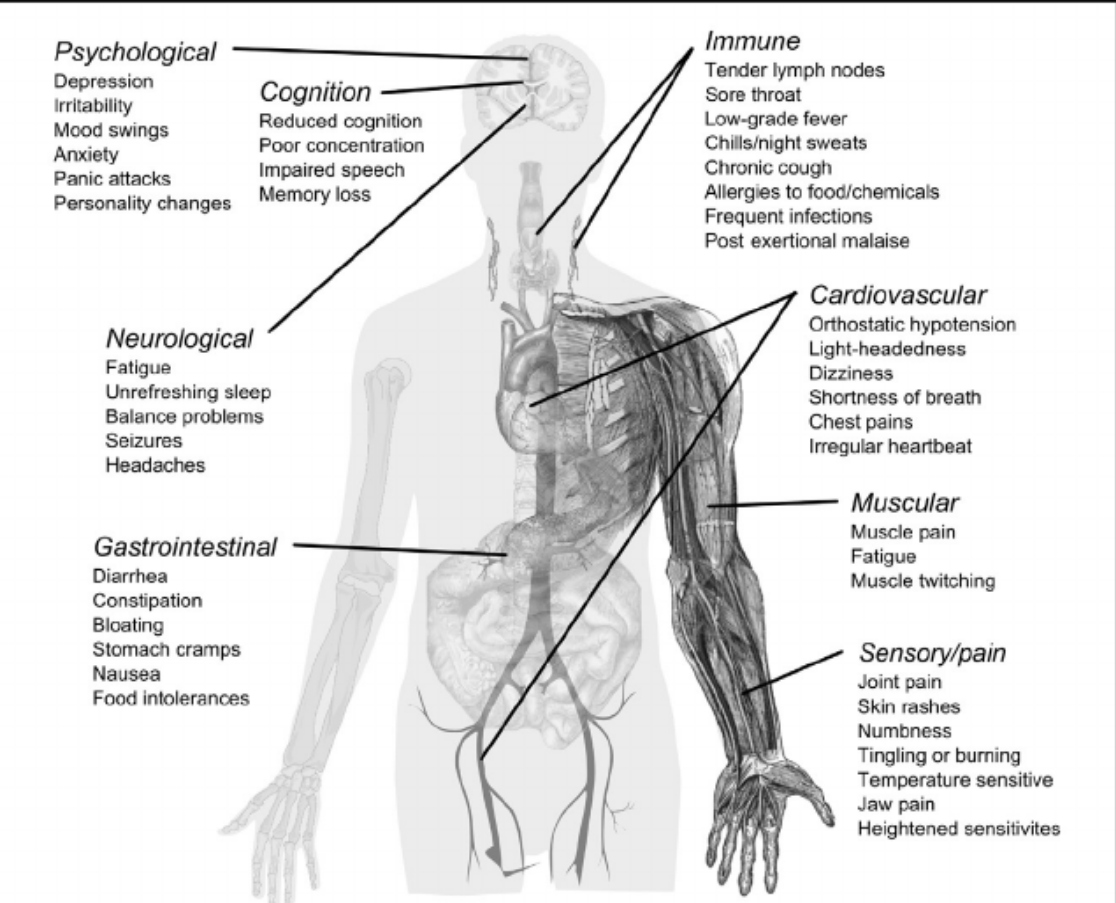
Although there is no consensus on the causes of ME/CFS, it is now agreed that there are
- Immune system
- Endocrine system
- Nervous system components.
This is a multisystem illness and there is multisystem involvement.
ME/CSF is costly to the individual and society. Many individuals are disabled. Given this occurs frequently in young people the length of their illness contributes to the costs. The hallmark of the disorder is the low functional activity of individuals often ( but not always) aggravated by physical activities. Many are unable to work resulting in social isolation. There are many unmet medical and social needs.
ME/CSF – The illness
ME/CFS is a spectrum illness. Some people are only mildly affected while others are severely impacted. This illness is present in every society in the world and the estimate is 400/100,000 people. This makes the condition more common than multiple sclerosis. The frequency that the illness has not changed over time but it is becoming more frequently recognised. It is anticipated that the frequency of diagnosis will increase following the COVID-19 pandemic. Researchers are close to determining if the symptoms that occur in 30% of people recovering from COVID are the same or similar to those with ME/CSF.
There is considerable overlap in the diagnosis of ME/ CFS with Fibromyalgia (FM). Studies have shown 20–70% of patients with FM also meet the diagnostic criteria for ME/CFS, while 35–75% of those with ME/ CFS also have FM.
A defining feature of ME/CSF is post-exertion malaise, or PEM, which is a worsening of neuro-immune symptoms caused by exertion. It is not understood why symptoms worsen with exertion, but one reason could be that the anaerobic threshold is substantially lower in people with ME/CFS, which means that fuel “burns” inefficiently much of the time. The effect is often described as feeling like having run a marathon, even when only minimal activity has been performed. The brain uses 20% of the body’s energy so cognitive processes of thinking, reading, talking can cause the same feelings and “brain fog”. The measurement of energy metabolism in any one individual is difficult and very few health practitioners appreciate the fact that energy metabolism is severely impaired in ME/CFS patients.
ME/CSF – The disease
10 years ago there was a strong debate as to whether this was an illness or a psychosomatic disorder. There is no longer any debate. ME/CFS is a multi-system illness characterised by a diverse range of debilitating symptoms.
The structural and functional neurological changes in the brains of individuals with ME/CFS can be measured by neuroimaging techniques.
Inflammation of the brain has been reported. While the underlying cause of this neuroinflammation in ME/CFS is unknown, overactivity of neurons resulting in the production of proinflammatory cytokines, reactive oxygen species and nitrogen species have been proposed as a potential mechanism.
The most common changes occur within the cortical regions of the brain. The cortical regions are important for higher-order processing and include the cingulate cortex The cingulate region has broad roles in emotional, cognitive and disruptions to working memory. Dysfunction in other areas of the brain correlates with increased mental fatigue, general fatigue and reduced activity.
Overall, these neuroimaging techniques confirm widespread disruption of the autonomic nervous system network including structural changes to the white matter of the brain and to neuronal connectivity. However, these findings are not consistent across various studies and as yet the cause of these anomalies remain unknown.
There are many immune system abnormalities that vary from one individual to the next. The most common biological marker is impaired natural killer cell function. Other markers such as micro RNAs are being studied. There is a strong possibility that the immunological abnormalities trigger glial cell inflammation( brain). There are over 5000 peer-reviewed articles attempting to unravel these issues.
Genetics
In many individuals, there is a genetic predisposition that can be triggered by an infection or trauma or stress or a toxin. This sets off a chain reaction that is mediated by changes in the endocrine and immunological systems resulting in sets of symptoms that make up the ME/CSF syndrome.
Treatment

Untreated the prognosis is poor however treatments that encompass biopsychosocial perspectives do improve the prognosis and quality of life.
The Pathways To Wellbeing program is a beneficial template to follow. For most individuals, recovery is a journey of discovery along many paths.
Recovery often requires discipline to explore various “path” as well as patience and persistence.
Most of the useful treatments to enhance the quality of living are based on lifestyle strategies.
Some of the carefully studied lifestyle strategies include nutritional modification, supplementation with prebiotics and probiotics, managing stress, finding an individually tailored and optimal amount of movement and exercise, (and in the majority avoiding aerobic exercise), enhancing sleep quality, energy pacing techniques as well as meditation and other strategies to manage the impact of living with a chronic illness. Pharmacological strategies to reduce brain inflammation and restore immune function are actively being tested.
High levels of personal hygiene to reduce the risk of infection and avoiding infection is an important but frequently forgotten strategy. COVID-19 has taught us the value of avoiding infections.
The recent interest in using immunosuppressive drugs has waned as the clinical trials have not met expectations. The search for solutions continues and perhaps one positive aspect of the COVID-19 pandemic is that it has generated a lot of research activity.
For many ME/CSF is a debilitating life-altering illness. Is it a permanent illness? My hope and respect for the scientific community is that the answer to this question will be…no.
Here is a lecture ( 1 hour) by Nancy Klimas, one of the key researchers.
