Pain is a complex phenomenon that has many sides to it and about which we still have much to learn. As a consequence there is much that is good and helpful to assist people with pain and there is also much that is based on myth and old wife’s tales.
Pain is a complex phenomenon that has many sides to it and about which we still have much to learn. As a consequence there is much that is good and helpful to assist people with pain and there is also much that is based on myth and old wife’s tales. In 1965, the Melzack &Wall’s Gate-Control Theory shed light on mechanisms in the central nervous system ( made up of the brain and spinal cord) that control the nerve impulses
carrying pain messages. Via a pain “gate” the brain and spinal cord are able to block or modify pain messages. This was the beginning of modern pain neuroscience.
In a typical acute injury, the brain and spinal cord “determine” the intensity and duration of the pain we experience as a result of tissue damage. Is the signals from the body a threat, if so it is registered as an unpleasant sensation … Pain. Here are examples to think about. There are times when a papercut is very painful and times when we see a bruise on the leg but do not know when or how the tissue damage occurs.
For reasons which are as yet unknown if the pain stimulus is intense and prolonged, then permanent changes in the structure and function of the spinal cord may occur leading to chronic persisting pain even after the tissue damage of an acute injury has resolved.
It is now known that the brain generates the experience of pain. This can occur whether there is tissue damage or not. This is the new knowledge of the last 15 or so years.
 An individual’s response to pain can be magnified and or maintained by having had previous painful experiences or by the expectation of pain and suffering.
An individual’s response to pain can be magnified and or maintained by having had previous painful experiences or by the expectation of pain and suffering.
Any form of stress can amplify pain. The body has many stress management systems which include nerves, hormones and emotional responses. These are all influenced to some extent by our genetic makeup.
The intensity of chronic pain frequently bears little or no relationship to the degree of the tissue injury. In some individuals there is no evidence of injury but intense pain. In other individuals
there is a lot of evidence of tissue damage but minimal or no pain.
We now have more knowledge and “tools” to assist individuals to understand the nature of their pain and to develop skills to live well with a pain that won’t go away.
A common myth- the two sided model of pain
The most common of these myth’s is the two sided model of pain that it is either “real” or that it is “all in the mind” and this simplistic understanding of pain causes much wasted effort and misdirected treatment.
A useful pain model
The following model is a simple way to understand the multiple factors involved in the pain that people experience from many different causes including arthritis.
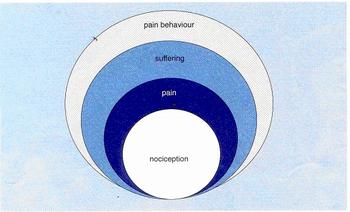 Nociception:
Nociception:
Refers to the electrical impulses generated by nerve endings.
It is only when those impulses reach the brain and are received by a wide variety of brain networks ( 800 at the last count) that the sensation are experienced.
We feel the sensations of
- throbbing, sore, aching, sharp, dull etc which we call pain. These sensations are the output of the brain. Change the brain…change the pain.
Pain:
Overlying the experience of pain is the conscious and subconscious interpretations of pain. It is the judgments about what casued it that often leads to the pathway of suffering.
Suffering:
Depending on the interpretation made by the person as to the cause of the pain and the intensity of the sensation, the degree of distress varies from one time to another.
The less the person perceives they have control over the pain the more intense the suffering is likely to be. This is the emotional aspect of pain and is the most obvious aspect of pain when the person experiences significant distress.
Pain Behaviour:
Pain behaviour is the way a person communicates to others that they are in pain. Pain behaviour can be appropriate or inappropriate.
There are numerous issues that influence the level of suffering and pain behaviour. They include:-
- the perceived intensity of the physical sensation
- the cause of the pain
- the context in which the pain is experienced
- the impact the pain has on their lives
Acute pain vs Chronic Pain:
Acute pain refers to short term pain of less than three months duration.
Chronic pain refers to pain that has continued beyond three months and as it continues, the psychological issues of the response and the management of pain, become more important.
In acute pain we focus on the likely trigger for the nociception ( the electrical signals from the nerve endings). Are there signs of inflammation or mechanical stress in the tissues?
Chronic pain occurs when there is persistence of the experience of pain? The nerve signals that result in the expereience of pain can be generated in the periphery, the spinal cord or the brain( central nervous system).
The pain itself becomes a problem in addition to the injury/illness that initiated it.
Pain Management:
People are familiar with the term “pain management” and the concept of whether a person is “coping “ is commonly used but what do these terms mean.
Pain management is often associated with the myth (or hope) that it means getting rid of the pain entirely and when I am referred off for pain management, I will return with no pain.
What is pain management?
Pain management means learning the skills that enable you to obtain a sense of control over the pain and to reduce the level of distress associated with it.
The issue of control is a central one in the management of pain. Pain management is a process of learning to achieve a sense of control over the experience.
- It may mean being able to reduce the intensity of the physical sensation,
- •learning to reduce the level of distress
- •or both.
Most people think in concrete terms about pain management with the view that it is about reducing the amount of pain (nociception) so that they can return to much of their
previous lifestyle.
In many cases however, pain management is about learning to cope with ongoing symptoms and restrictions with minimal distress and being able to adapt practically and psychologically to this.I t is about developing a health tolerance to uncertainty and be willing to explore may different approaches.
What can I do for myself?Inherent in this term is the notion that the person in pain will take some responsibility in learning what is required to gain this control. Some pain management is administered by
- doctors in the form of medication and non drug therapies
- •other health practitioners
- complementary health practitioners
but much of what is required in pain management must come from the person themselves and requires a willingness and motivation to do so.
Coping:
Coping is a loose notion that means different things to different people. It does not mean experiencing no distress at all.
It is rare that a person in chronic pain reaches a state where they experience no distress. It means
- not allowing the pain to overwhelm them or to limit their lives is such a way that it diminishes the quality of life.
- maintaining as much activity and involvement in life as possible
- not allowing depression, anger or anxiety to be an issue in their lives.
What is important/What works
The major component of managing pain is the person’s psychological response to the pain and the impact that it has on their lives.
For many people learning to cope with a chronic illness/injury is a journey that takes time to master.
The initial response is to pursue medical treatments looking for a solution to the pain and this is very appropriate as good medical advice and management is essential.
In the longer term psychological assistance and understanding as well as comprehensive pain management skills are vital aspects of treatment.
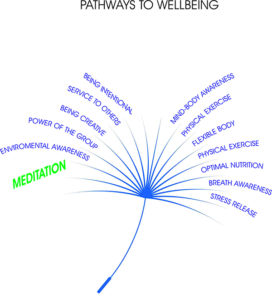 The classic ongoing pain management techniques of
The classic ongoing pain management techniques of
- appropriate exercise
- medication
- self help strategies ie use of heat and or ice, hot baths
- relaxation techniques
- meditation
- and of seeking asssistance from therapists
are very helpful and necessary.
While a person continues to look to others to resolve their pain they will be reluctant participants in activities that require them to self manage their condition.
Sometimes the combination of educational input and encouragement to utilise such techniques assists a person to learn that they are able to gain some control over the pain.
Much of the distress that occurs is attributable to the person feeling that they have little or no control over the pain or its consequences. This is especially true when the person
has tried all they know and continues to experience a significant amount of pain.
The focus of pain management is to reduce the distress and encourage the person to think practically about the steps they can take to control their pain. The shift from reliance on others
(especially the medical profession) to learning what the person can do for themselves is an i mportant one.
This shift opens up a wide range of techniques and strategies that the person can explore and work with.
Key Steps to take control.
- Education about pain/injury/illness – addressing the understanding the person has about pain, injury and illness and their beliefs about pain. Inaccurate beliefs may lead to a self defeating response to the pain i.e. excessive rest, excessive use of medication.
- Appropriate use of medication – analgesic, anti-inflammatories, anti-depressants, muscle relaxants, anti-anxietants, steroids etc. Ensuring that medication use is limited and that the person does not get into a habit of taking the medication whether they need to or not. Is it helping or is it just a crutch? If a medication does not lead to a higher quality of life then it is of no use.
- Ice/heat – hot water bottles, heat packs, heat pads, electric blankets, hot towels, heated pools, baths, spas, showers, ice, cold packs etc.
- TENS – Transcutaneous Electrical Nerve Stimulation
- Exercise/Stretching – addressing the issue of how much exercise and how much pain to tolerate when exercising.
- Relaxation/Meditation/Self Hypnosis/Visualisation – Use of a variety of techniques to reduce muscle tension and distress. Using self managed techniques or CD’s etc. This ia a much underatted and used skill.
- Cognitive skills including distraction and self talk. What is the person telling themselves about the pain generally and/or specifically about a particular difficult situation. Is it helpful, positive and does it assist them or does it add to their distress.
- Ergonomics, pacing – Ensuring that the environment is adapted to the needs of the person in pain and that they learn to pace their activities to avoid severe pain episodes and conserve energy for coping with the pain.
- Sleep skills – relaxation, distraction, medication, getting comfortable, cognitive skills (don’t awfulise and put pressure on to go to sleep) For how to sleep well click here>>>
- Physically appropriate activities – purposeful, meaningful activities that provide a sense of enjoyment, fulfilment and self esteem. One of the basic approaches to pain management is to ensure that the person remains as involved in their normal lifestyle as possible.
The skills that help one person aren’t the skills that assist another and so each person must find those things that are helpful and provide them with a sense of control. Practice with most of these techniques is important and the more a person practices the more helpful these techniques will be.
;
Chronic pain can be manged without opioids.
Here is an excellent article and You Tube http://tinyurl.com/hc6ubdq